A frailty index is rationing treatment for older and disabled people who catch coronavirus. We are not sacrificial lambs
Lockdown was easy for me, it has become my daily state more frequently throughout my life. I have a debilitating connective tissue disorder that keeps me indoors most days. It was a relief I no longer had to go out and pretend to be normal when wracked with ill-health and hidden pain. Like thousands of others with rare conditions, I’m already in a minority within a minority, marginalised by our NHS, battling increasing disability day by day. So, while many fear a second lockdown over the winter months, I haven’t gone out more often since the first one was lifted because I risk a double jeopardy – catching Covid, then being a low priority for medical care.
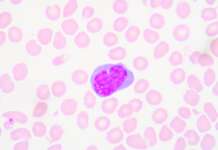
Back in March, without consultation and days before the first lockdown, the Clinical Frailty Scale (CFS), a worldwide tool used to swiftly identify frailty in older patients to improve acute care, was adapted by the National Institute for Health and Care Excellence (Nice). It asked NHS staff in England to score the frailty of Covid patients. Rather than aiming to improve care, it seems the CFS – a fitness-to-frailty sheet using scores from one to nine – was used to work out which patients should be denied acute care. Nice’s new guidelines advised NHS trusts to “sensitively discuss a possible ‘do not attempt cardiopulmonary resuscitation’ decision with all adults with capacity and an assessment suggestive of increased frailty”.