Image copyright
Getty Images
The coronavirus emerged in only December last year, but already the world is dealing with a pandemic of the virus and the disease it causes – Covid-19.
For most, the disease is mild, but some people die.
So how is the virus attacking the body, why are some people being killed and how is it treated?
Incubation period
This is when the virus is establishing itself.
Viruses work by getting inside the cells your body is made of and then hijacking them.
The coronavirus, officially called Sars-CoV-2, can invade your body when you breathe it in (after someone coughs nearby) or you touch a contaminated surface and then your face.
It first infects the cells lining your throat, airways and lungs and turns them into “coronavirus factories” that spew out huge numbers of new viruses that go on to infect yet more cells.
At this early stage, you will not be sick and some people may never develop symptoms.
The incubation period, the time between infection and first symptoms appearing, varies widely, but is five days on average.
Media playback is unsupported on your device
Mild disease
This is all most people will experience.
Covid-19 is a mild infection for eight out of 10 people who get it and the core symptoms are a fever and a cough.
Body aches, sore throat and a headache are all possible, but not guaranteed.
The fever, and generally feeling grotty, is a result of your immune system responding to the infection. It has recognised the virus as a hostile invader and signals to the rest of the body something is wrong by releasing chemicals called cytokines.
These rally the immune system, but also cause the body aches, pain and fever.
The coronavirus cough is initially a dry one (you’re not bringing stuff up) and this is probably down to irritation of cells as they become infected by the virus.
Some people will eventually start coughing up sputum – a thick mucus containing dead lung cells killed by the virus.
These symptoms are treated with bed rest, plenty of fluids and paracetamol. You won’t need specialist hospital care.
This stage lasts about a week – at which point most recover because their immune system has fought off the virus.
However, some will develop a more serious form of Covid-19.
This is the best we understand at the moment about this stage, however, there are studies emerging that suggest the disease can cause more cold-like symptoms such as a runny nose too.
Severe disease
If the disease progresses it will be due to the immune system overreacting to the virus.
Those chemical signals to the rest of the body cause inflammation, but this needs to be delicately balanced. Too much inflammation can cause collateral damage throughout the body.
“The virus is triggering an imbalance in the immune response, there’s too much inflammation, how it is doing this we don’t know,” said Dr Nathalie MacDermott, from King’s College London.
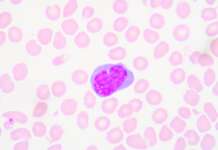
Image copyright
SPL
Scans of lungs infected with coronavirus showing areas of pneumonia
Inflammation of the lungs is called pneumonia.
If it was possible to travel through your mouth down the windpipe and through the tiny tubes in your lungs, you’d eventually end up in tiny little air sacs.
This is where oxygen moves into the blood and carbon dioxide moves out, but in pneumonia the tiny sacs start to fill with water and can eventually cause shortness of breath and difficulty breathing.
Some people will need a ventilator to help them breathe.
This stage is thought to affect around 14% of people, based on data from China.
Critical disease
It is estimated around 6% of cases become critically ill.
By this point the body is starting to fail and there is a real chance of death.
The problem is the immune system is now spiralling out of control and causing damage throughout the body.
It can lead to septic shock when the blood pressure drops to dangerously low levels and organs stop working properly or fail completely.
Acute respiratory distress syndrome caused by widespread inflammation in the lungs stops the body getting enough oxygen it needs to survive. It can stop the kidneys from cleaning the blood and damage the lining of your intestines.
“The virus sets up such a huge degree of inflammation that you succumb… it becomes multi-organ failure,” Dr Bharat Pankhania said.
And if the immune system cannot get on top of the virus, then it will eventually spread to every corner of the body where it can cause even more damage.
Treatment by this stage will be highly invasive and can include ECMO or extra-corporeal membrane oxygenation.
This is essentially an artificial lung that takes blood out of the body through thick tubes, oxygenates it and pumps it back in.
But eventually the damage can reach fatal levels at which organs can no longer keep the body alive.
The first deaths
Doctors have described how some patients died despite their best efforts.
The first two patients to die at Jinyintan Hospital in Wuhan, China, detailed in the Lancet Medical journal, were seemingly healthy, although they were long-term smokers and that would have weakened their lungs.
The first, a 61-year-old man, had severe pneumonia by the time he arrived at hospital.
He was in acute respiratory distress, and despite being put on a ventilator, his lungs failed and his heart stopped beating.
He died 11 days after he was admitted.
The second patient, a 69-year-old man, also had acute respiratory distress syndrome.
He was attached to an ECMO machine but this wasn’t enough. He died of severe pneumonia and septic shock when his blood pressure collapsed.
Follow James on Twitter.